Symdeko Prescribing Information
Package insert / product label
Generic name: tezacaftor and ivacaftor
Dosage form: kit
Drug class: CFTR combinations
Medically reviewed by Drugs.com. Last updated on Dec 1, 2022.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Patient Counseling Information
Indications and Usage for Symdeko
Symdeko is indicated for the treatment of cystic fibrosis (CF) in patients age 6 years and older who are homozygous for the F508del mutation or who have at least one mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene that is responsive to tezacaftor/ivacaftor based on in vitro data and/or clinical evidence [see Clinical Pharmacology (12.1) and Clinical Studies (14)].
If the patient’s genotype is unknown, an FDA-cleared CF mutation test should be used to detect the presence of a CFTR mutation followed by verification with bi-directional sequencing when recommended by the mutation test instructions for use.
Symdeko Dosage and Administration
General Dosing Information
Swallow the tablets whole.
Symdeko should be taken with fat-containing food, such as food recommended in standard nutritional guidelines. Examples of meals or snacks that contain fat are those prepared with butter or oils or those containing eggs, cheeses, nuts, whole milk, or meats, etc. [see Clinical Pharmacology (12.3)].
Recommended Dosage in Adults, Adolescents, and Children Age 6 Years and Older
Adults, adolescents, and children age 6 years and older should be dosed according to Table 1. The morning and the evening dose should be taken approximately 12 hours apart.
| Age | Morning (one tablet) |
Evening (one tablet) |
|---|---|---|
| 6 to <12 years weighing <30 kg | tezacaftor 50 mg/ivacaftor 75 mg | ivacaftor 75 mg |
| 6 to <12 years weighing ≥30 kg | tezacaftor 100 mg/ivacaftor 150 mg | ivacaftor 150 mg |
| ≥12 years | tezacaftor 100 mg/ivacaftor 150 mg | ivacaftor 150 mg |
Information for Missed Doses:
If 6 hours or less have passed since the missed morning or evening dose, the patient should take the missed dose as soon as possible and continue on the original schedule. If more than 6 hours have passed since the missed morning or evening dose, the patient should not take the missed dose. The next scheduled dose can be taken at the usual time. More than one dose should not be taken at the same time.
Recommended Dosage for Patients with Hepatic Impairment
For dose adjustment for patients with hepatic impairment, refer to Table 2.
Studies have not been conducted in patients with severe hepatic impairment (Child-Pugh Class C), but exposure of tezacaftor and ivacaftor is expected to be higher than in patients with moderate hepatic impairment. Therefore, Symdeko should be used with caution at an adjusted dose after weighing the risks and benefits of treatment in these patients [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
| Hepatic Impairment | Morning | Evening | |
|---|---|---|---|
| Patients Age 6 to <12 Years Weighing <30kg | Patients Age 6 to <12 Years Weighing ≥30 kg and Patients Age ≥12 Years | All Patients | |
| Mild (Child-Pugh Class A) | No dose adjustment | No dose adjustment | No dose adjustment |
| Moderate (Child-Pugh Class B) | One tablet of tezacaftor 50 mg/ivacaftor 75 mg once daily | One tablet of tezacaftor 100 mg/ivacaftor 150 mg once daily | No ivacaftor dose |
| Severe (Child-Pugh Class C) | One tablet of tezacaftor 50 mg/ivacaftor 75 mg once daily (or less frequently) |
One tablet of tezacaftor 100 mg/ivacaftor 150 mg once daily (or less frequently) |
Dosage Adjustment for Patients Taking Drugs that are CYP3A Inhibitors
The dosing regimen of Symdeko should be adjusted when co-administered with moderate and strong CYP3A inhibitors.
Moderate CYP3A inhibitors:
When co-administered with moderate CYP3A inhibitors (e.g., fluconazole, erythromycin), the dosing regimen should be adjusted as in Table 3 [see Drug Interactions (7.2), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
| Day 1 | Day 2 | Day 3 | Day 4* | |
|---|---|---|---|---|
|
||||
| Patients Age 6 to <12 Years Weighing <30 kg | ||||
| Morning | ||||
| Tezacaftor 50 mg/ivacaftor 75 mg tablet | ✓ | — | ✓ | — |
| Ivacaftor 75 mg tablet | — | ✓ | — | ✓ |
| Evening | ||||
| Ivacaftor 75 mg tablet | — | — | — | — |
| Patients Age 6 to <12 Years Weighing ≥30 kg and Patients Age ≥12 Years | ||||
| Morning | ||||
| Tezacaftor 100 mg/ivacaftor 150 mg tablet | ✓ | — | ✓ | — |
| Ivacaftor 150 mg tablet | — | ✓ | — | ✓ |
| Evening | ||||
| Ivacaftor 150 mg tablet | — | — | — | — |
Strong CYP3A inhibitors:
When co-administered with strong CYP3A inhibitors (e.g., ketoconazole, itraconazole, posaconazole, voriconazole, telithromycin, and clarithromycin), the dosing regimen should be adjusted as in Table 4 [see Drug Interactions (7.2), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
| Day 1 | Day 2 and Day 3 | Day 4* | |
|---|---|---|---|
|
|||
| Patients Age 6 to <12 Years Weighing <30 kg | |||
| Morning | |||
| Tezacaftor 50 mg/ivacaftor 75 mg tablet | ✓ | — | ✓ |
| Evening† | |||
| Ivacaftor 75 mg tablet | — | — | — |
| Patients Age 6 to <12 Years Weighing ≥30 kg and Patients Age ≥12 Years | |||
| Morning | |||
| Tezacaftor 100 mg/ivacaftor 150 mg tablet | ✓ | — | ✓ |
| Evening† | |||
| Ivacaftor 150 mg tablet | — | — | — |
Food or drink containing grapefruit should be avoided during treatment with Symdeko [see Drug Interactions (7.2) and Patient Counseling Information (17)].
Dosage Forms and Strengths
Tablets: Tezacaftor 50 mg/ivacaftor 75 mg fixed-dose combination tablets co-packaged with ivacaftor 75 mg tablets
- Tezacaftor 50 mg/ivacaftor 75 mg tablets are white, capsule-shaped, and debossed with «V50» on one side and plain on the other.
- Ivacaftor 75 mg tablets are light blue, capsule-shaped, and printed with «V 75» in black ink on one side and plain on the other.
Tablets: Tezacaftor 100 mg/ivacaftor 150 mg fixed-dose combination tablets co-packaged with ivacaftor 150 mg tablets
- Tezacaftor 100 mg/ivacaftor 150 mg tablets are yellow, capsule-shaped, and debossed with «V100» on one side and plain on the other.
- Ivacaftor 150 mg tablets are light blue, capsule-shaped, and printed with «V 150» in black ink on one side and plain on the other.
Contraindications
None.
Warnings and Precautions
Transaminase (AST/ALT) Elevations
Elevated transaminases have been observed in patients with CF treated with Symdeko, as well as with ivacaftor monotherapy. Assessments of transaminases (ALT and AST) are recommended for all patients prior to initiating Symdeko, every 3 months during the first year of treatment, and annually thereafter. For patients with a history of transaminase elevations more frequent monitoring should be considered. In the event of significant elevations of transaminases, e.g., patients with ALT or AST >5 × upper limit of normal (ULN), or ALT or AST >3 × ULN with bilirubin >2 × ULN, dosing should be interrupted and laboratory tests closely followed until the abnormalities resolve. Following the resolution of transaminase elevations consider the benefits and risks of resuming treatment [see Adverse Reactions (6)].
Concomitant Use with CYP3A Inducers
Exposure to ivacaftor is significantly decreased and exposure to tezacaftor may be reduced by the concomitant use of CYP3A inducers, which may reduce the therapeutic effectiveness of Symdeko. Therefore, co-administration with strong CYP3A inducers is not recommended [see Drug Interactions (7.1), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
Cataracts
Cases of non-congenital lens opacities have been reported in pediatric patients treated with Symdeko, as well as with ivacaftor monotherapy. Although other risk factors were present in some cases (such as corticosteroid use, exposure to radiation), a possible risk attributable to treatment with Symdeko cannot be excluded. Baseline and follow-up ophthalmological examinations are recommended in pediatric patients initiating treatment with Symdeko [see Use in Specific Populations (8.4) and Patient Counseling Information (17)].
Adverse Reactions
The following adverse reactions are discussed in greater detail in other sections of the label:
- Transaminase Elevations [see Warnings and Precautions (5.1)]
- Cataracts [see Warnings and Precautions (5.3)]
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The overall safety profile of Symdeko is based on data from 1001 patients in three double-blind, placebo-controlled, clinical trials: two parallel-group trials of 12 and 24 week duration and one cross-over design trial of 8 weeks duration. Eligible patients were also able to participate in an open-label extension safety study (up to 96 weeks of Symdeko). In the three placebo-controlled trials (Trials 1, 2, and 3), a total of 496 patients with CF age 12 years and older received at least one dose of Symdeko. The proportion of patients who discontinued study drug prematurely due to adverse reactions was 1.6% for Symdeko-treated patients and 2.0% for placebo-treated patients. Serious adverse reactions, whether considered drug-related or not by the investigators, that occurred more frequently in Symdeko-treated patients compared to placebo included distal intestinal obstruction syndrome, 3 (0.6%) Symdeko-treated patients vs. 0 placebo. There were no deaths in the placebo-controlled trials, and one death in the open label extension study due to respiratory failure and influenza infection in a patient who had discontinued Symdeko seven weeks prior.
The safety profile of Symdeko was generally similar across all subgroups of patients, including analysis by age, sex, baseline percent predicted FEV1 (ppFEV1), and geographic regions.
Table 5 shows adverse reactions occurring in ≥3% of Symdeko-treated patients that also occurred at a higher rate than in the placebo-treated patients in the 12- and 24-week placebo controlled, parallel-group trials (Trials 1 and 3).
| Adverse Reactions (Preferred Term) | Symdeko N=334 n (%) |
Placebo N=343 n (%) |
|---|---|---|
| Headache | 49 (15) | 44 (13) |
| Nausea | 29 (9) | 24 (7) |
| Sinus congestion | 13 (4) | 6 (2) |
| Dizziness | 12 (4) | 8 (2) |
The safety data from the following trials are similar to that observed in Trials 1 and 3:
- an 8-week randomized, double-blind, placebo-controlled crossover study in 244 patients with CF age 12 years and older who were heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor (Trial 2).
- a 24-week open-label study in 70 patients with CF age 6 to less than 12 years who were either homozygous for the F508del mutation or heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor (Trial 4).
Laboratory abnormalities
Transaminase elevations
During the placebo-controlled trials in patients age 12 years and older, the incidence of maximum transaminase (ALT or AST) >8, >5, and >3 × the upper limit of normal (ULN) was similar between Symdeko-treated patients and placebo-treated patients; 0.2%, 1.0%, and 3.4% in Symdeko-treated patients, and 0.4%, 1.0%, and 3.4% in placebo-treated patients. One patient (0.2%) on Symdeko and 2 patients (0.4%) on placebo permanently discontinued treatment for elevated transaminases. No Symdeko-treated patients experienced a transaminase elevation >3 × ULN associated with elevated total bilirubin >2 × ULN.
During the 24-week, open-label study in patients age 6 to less than 12 years (Trial 4), the incidence of maximum transaminase (ALT or AST) >8, >5, and >3 × ULN were 1.4%, 4.3%, and 10.0%, respectively. No Symdeko-treated patients experienced a transaminase elevation >3 × ULN associated with elevated total bilirubin >2 × ULN or discontinued Symdeko treatment due to transaminase elevations.
Drug Interactions
Potential for other drugs to affect tezacaftor/ivacaftor
Inducers of CYP3A
Tezacaftor and ivacaftor are substrates of CYP3A (ivacaftor is a sensitive substrate of CYP3A). Concomitant use of CYP3A inducers may result in reduced exposures and thus reduced Symdeko efficacy. Co-administration of ivacaftor with rifampin, a strong CYP3A inducer, significantly decreased ivacaftor exposure (area under the curve [AUC]) by 89%. Tezacaftor exposures can also be expected to decrease significantly during co-administration with strong CYP3A inducers. Therefore, co-administration of Symdeko with strong CYP3A inducers is not recommended [see Warnings and Precautions (5.2), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
Examples of strong CYP3A inducers include:
- rifampin, rifabutin, phenobarbital, carbamazepine, phenytoin, and St. John’s wort (Hypericum perforatum)
Inhibitors of CYP3A
Co-administration with itraconazole, a strong CYP3A inhibitor, increased tezacaftor exposure (AUC) by 4.0-fold and ivacaftor by 15.6-fold. When co-administered with strong CYP3A inhibitors, the dosing regimen of Symdeko should be adjusted [see Dosage and Administration (2.4), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
Examples of strong CYP3A inhibitors include:
- ketoconazole, itraconazole, posaconazole, and voriconazole
- telithromycin and clarithromycin
Co-administration of fluconazole increased ivacaftor exposure (AUC) by 3.0-fold. Simulation suggested co-administration with fluconazole, a moderate CYP3A inhibitor, may increase tezacaftor exposure (AUC) by approximately 2.0-fold. When co-administered with moderate CYP3A inhibitors, the dosing regimen of Symdeko should be adjusted [see Dosage and Administration (2.4), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
Examples of moderate CYP3A inhibitors include:
- fluconazole
- erythromycin
Co-administration of Symdeko with grapefruit juice, which contains one or more components that moderately inhibit CYP3A, may increase exposure of tezacaftor and ivacaftor; therefore, food or drink containing grapefruit should be avoided during treatment with Symdeko [see Dosage and Administration (2.4), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
Ciprofloxacin
Co-administration of Symdeko with ciprofloxacin had no significant effect on the exposure of tezacaftor or ivacaftor. Therefore, no dose adjustment is necessary during concomitant administration of Symdeko with ciprofloxacin [see Clinical Pharmacology (12.3)].
Potential for tezacaftor/ivacaftor to affect other drugs
CYP3A Substrates
Co-administration of Symdeko with midazolam (oral), a sensitive CYP3A substrate, did not affect midazolam exposure. No dose adjustment of CYP3A substrates is required when co-administered with Symdeko [see Clinical Pharmacology (12.3)].
CYP2C9 Substrates
Ivacaftor may inhibit CYP2C9; therefore, monitoring of the international normalized ratio (INR) during co administration of Symdeko with warfarin is recommended. Other medicinal products for which exposure may be increased by Symdeko include glimepiride and glipizide; these medicinal products should be used with caution [see Clinical Pharmacology (12.3)].
Digoxin and Other P-gp Substrates
Co-administration of Symdeko with digoxin, a sensitive P-gp substrate, increased digoxin exposure by 1.3-fold consistent with weak inhibition of P-gp by ivacaftor. Administration of Symdeko may increase systemic exposure of medicinal products that are sensitive substrates of P-gp, which may increase or prolong their therapeutic effect and adverse reactions. When used concomitantly with digoxin or other substrates of P-gp with a narrow therapeutic index such as cyclosporine, everolimus, sirolimus, and tacrolimus, caution and appropriate monitoring should be used [see Clinical Pharmacology (12.3)].
Hormonal Contraceptives
Symdeko has been studied with an ethinyl estradiol/norethindrone oral contraceptive and was found to have no significant effect on the exposures of the hormonal contraceptive. Symdeko is not expected to modify the efficacy of hormonal contraceptives [see Clinical Pharmacology (12.3)].
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
There are limited and incomplete human data from clinical trials and post-marketing reports on the use of Symdeko or its individual components, tezacaftor and ivacaftor, in pregnant women to inform a drug-associated risk. Although there are no animal reproduction studies with the concomitant administration of tezacaftor and ivacaftor, separate reproductive and developmental studies were conducted with tezacaftor and ivacaftor in pregnant rats and rabbits. In animal reproduction studies, oral administration of tezacaftor to pregnant rats and rabbits during organogenesis demonstrated no teratogenicity or adverse developmental effects at doses that produced maternal exposures up to approximately 3 times the exposure at the maximum recommended human dose (MRHD) in rats and 0.2 times the MRHD in rabbits (based on summed AUCs for tezacaftor and M1 metabolite). Oral administration of ivacaftor to pregnant rats and rabbits during organogenesis demonstrated no teratogenicity or adverse developmental effects at doses that produced maternal exposures up to approximately 6 and 16 times the exposure at the MRHD, respectively. No adverse developmental effects were observed after oral administration of either tezacaftor or ivacaftor to pregnant rats from the period of organogenesis through lactation at doses that produced maternal exposures approximately 1 and 4 times the exposures at the MRHD, respectively (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
Tezacaftor
In an embryo-fetal development study in pregnant rats dosed during the period of organogenesis from gestation Days 6-17, tezacaftor was not teratogenic and did not affect fetal development or survival at exposures up to 3 times the MRHD (based on summed AUCs for tezacaftor and M1 metabolite at maternal oral doses up to 100 mg/kg/day). In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis from gestation Days 7-20, tezacaftor was not teratogenic and did not affect fetal development or survival at exposures up to 0.2 times the MRHD (based on summed AUCs for tezacaftor and M1 metabolite at maternal oral doses up to 25 mg/kg/day). Lower fetal body weights were observed in rabbits at a maternally toxic dose that produced exposures approximately 1 times the MRHD (at a maternal dose of 50 mg/kg/day). In a pre- and postnatal development (PPND) study in pregnant rats dosed from gestation Day 6 through lactation Day 18, tezacaftor had no adverse developmental effects on pups at an exposure of approximately 1 times the MRHD (based on summed AUCs for tezacaftor and M1 metabolite at a maternal dose of 25 mg/kg/day). Decreased fetal body weights and early developmental delays in pinna detachment, eye opening, and righting reflex occurred at a maternally toxic dose (based on maternal weight loss) that produced exposures approximately 2 times the exposure at the MRHD (based on summed AUCs for tezacaftor and M1 metabolite at a maternal oral dose of 50 mg/kg/day). Placental transfer of tezacaftor was observed in pregnant rats.
Ivacaftor
In an embryo-fetal development study in pregnant rats dosed during the period of organogenesis from gestation Days 7-17, ivacaftor was not teratogenic and did not affect fetal survival at exposures up to 6 times the MRHD (based on summed AUCs for ivacaftor and its metabolites at a maternal oral dose of 200 mg/kg/day). In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis from gestation Days 7-19, ivacaftor was not teratogenic and did not affect fetal development or survival at exposures up to 16 times the MRHD (on an ivacaftor AUC basis at maternal oral doses up to 100 mg/kg/day). In a PPND study in pregnant rats dosed from gestation Day 7 through lactation Day 20, ivacaftor had no effects on delivery or growth and development of offspring at exposures up to 4 times the MRHD (based on summed AUCs for ivacaftor and its metabolites at maternal oral doses up to 100 mg/kg/day). Decreased fetal body weights were observed at a maternally toxic dose that produced exposures 6 times the MRHD. Placental transfer of ivacaftor was observed in pregnant rats and rabbits.
Lactation
Risk Summary
There is no information regarding the presence of tezacaftor or ivacaftor in human milk, the effects on the breastfed infant, or the effects on milk production. Both tezacaftor and ivacaftor are excreted into the milk of lactating rats (see Data). The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Symdeko and any potential adverse effects on the breastfed child from Symdeko or from the underlying maternal condition.
Data
Tezacaftor
Lacteal excretion of tezacaftor in rats was demonstrated following a single oral dose (30 mg/kg) of 14C-tezacaftor administered 6 to 10 days postpartum to lactating dams. Exposure of 14C-tezacaftor in milk was approximately 3 times higher than in plasma (based on AUC0-72h).
Ivacaftor
Lacteal excretion of ivacaftor in rats was demonstrated following a single oral dose (100 mg/kg) of 14C-ivacaftor administered 9 to 10 days postpartum to lactating dams. Exposure of 14C-ivacaftor in milk was approximately 1.5 times higher than in plasma (based on AUC0-24h).
Pediatric Use
The safety and effectiveness of Symdeko for the treatment of CF have been established in pediatric patients age 6 to less than 18 years who are homozygous for the F508del mutation or who have at least one mutation in the CFTR gene that is responsive to tezacaftor/ivacaftor based on in vitro data and/or clinical evidence [see Clinical Pharmacology (12.1) and Clinical Studies (14)].
Clinical trials included the following patients with CF:
- 12 to less than 18 years of age who are homozygous for the F508del mutation [see Adverse Reactions (6) and Clinical Studies (14)].
- 12 to less than 18 years of age who are heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor [see Adverse Reactions (6) and Clinical Studies (14)].
- 6 to less than 12 years of age who are either homozygous for the F508del mutation or heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor [see Adverse Reactions (6) and Clinical Pharmacology (12)]
The effectiveness of Symdeko in patients age 6 to less than 12 years was extrapolated from patients age 12 years and older with support from population pharmacokinetic analyses showing similar tezacaftor and ivacaftor exposure levels in patients age 6 to less than 12 years and in patients age 12 years and older [see Clinical Pharmacology (12.3)]. Safety of Symdeko in this population was derived from a 24-week, open-label, clinical trial in 70 patients age 6 to less than 12 years (mean age at screening 8.1 years) administered either tezacaftor 50 mg/ivacaftor 75 mg and ivacaftor 75 mg or tezacaftor 100 mg/ivacaftor 150 mg and ivacaftor 150 mg, 12 hours apart (Trial 4). The safety profile for patients in this trial was similar to that observed in Trials 1 and 3 [see Adverse Reactions (6.1)].
The safety and effectiveness of Symdeko in patients with CF younger than 6 years of age have not been studied.
Juvenile Animal Toxicity Data
Findings of cataracts were observed in juvenile rats dosed from postnatal Day 7 through 35 with ivacaftor dose levels of 10 mg/kg/day and higher (0.25 times the MRHD based on systemic exposure of ivacaftor and its metabolites). This finding has not been observed in older animals.
Geriatric Use
Clinical trials of Symdeko did not include sufficient numbers of patients 65 years of age and over to determine whether they respond differently from younger patients.
Hepatic Impairment
No dose adjustment is necessary for patients with mild hepatic impairment (Child-Pugh Class A). A reduced dose of Symdeko is recommended in patients with moderate hepatic impairment (Child-Pugh Class B). There is no experience in patients with severe hepatic impairment (Child-Pugh Class C), but tezacaftor/ivacaftor exposure is expected to be higher than in patients with moderate hepatic impairment. Therefore, use with caution at a reduced dose in patients with severe hepatic impairment after weighing the risks and benefits of treatment [see Dosage and Administration (2.3), Clinical Pharmacology (12.3), and Patient Counseling Information (17)].
Renal Impairment
Symdeko has not been studied in patients with moderate or severe renal impairment or in patients with end-stage renal disease. No dose adjustment is recommended for mild and moderate renal impairment. Caution is recommended in patients with severe renal impairment or end-stage renal disease [Clinical Pharmacology (12.3)].
Patients with Severe Lung Dysfunction
Trial 1 and Trial 2 included a total of 39 Symdeko-treated patients with ppFEV1 <40 at baseline (range 30-40); 23 patients in Trial 1 and 16 patients in Trial 2. There were 24 placebo-treated patients in Trial 1, and 15 placebo- and 13 ivacaftor-treated patients in Trial 2, with ppFEV1 <40 at baseline. The safety and efficacy in this subgroup were comparable to the overall results observed in both Trials 1 and 2.
Overdosage
No specific antidote is available for overdose with Symdeko. Treatment of overdosage consists of general supportive measures including monitoring of vital signs and observation of the clinical status of the patient.
Symdeko Description
Symdeko is co-packaged as a tezacaftor/ivacaftor fixed-dose combination tablet and an ivacaftor tablet. Both tablets are for oral administration.
Tezacaftor 50 mg/ivacaftor 75 mg fixed-dose combination tablets and ivacaftor 75 mg tablets:
The tezacaftor/ivacaftor fixed-dose combination tablet is available as a white, capsule-shaped, film-coated tablet containing 50 mg of tezacaftor, 75 mg of ivacaftor, and the following inactive ingredients: croscarmellose sodium, hypromellose, hypromellose acetate succinate, magnesium stearate, microcrystalline cellulose and sodium lauryl sulfate. The tablet film coat contains HPMC/hypromellose 2910, hydroxypropyl cellulose, talc and titanium dioxide.
The ivacaftor tablet is available as a light blue, capsule-shaped, film-coated tablet containing 75 mg of ivacaftor and the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The tablet film coat contains carnauba wax, FD&C Blue #2, PEG 3350, polyvinyl alcohol, talc, and titanium dioxide. The printing ink contains ammonium hydroxide, iron oxide black, propylene glycol, and shellac.
Tezacaftor 100 mg/ivacaftor 150 mg fixed-dose combination tablets and ivacaftor 150 mg tablets:
The tezacaftor/ivacaftor fixed-dose combination tablet is available as a yellow, capsule-shaped, film-coated tablet containing 100 mg of tezacaftor, 150 mg of ivacaftor, and the following inactive ingredients: croscarmellose sodium, hypromellose, hypromellose acetate succinate, magnesium stearate, microcrystalline cellulose and sodium lauryl sulfate. The tablet film coat contains HPMC/hypromellose 2910, hydroxypropyl cellulose, iron oxide yellow, talc and titanium dioxide.
The ivacaftor tablet is available as a light blue, capsule-shaped, film-coated tablet containing 150 mg of ivacaftor and the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The tablet film coat contains carnauba wax, FD&C Blue #2, PEG 3350, polyvinyl alcohol, talc, and titanium dioxide. The printing ink contains ammonium hydroxide, iron oxide black, propylene glycol, and shellac.
The active ingredients of Symdeko are described below.
Tezacaftor
Tezacaftor is a white to off-white powder that is practically insoluble in water (<5 microgram/mL). Its chemical name of tezacaftor is 1-(2,2-difluoro-2H-1,3-benzodioxol-5-yl)-N-{1-[(2R)-2,3-dihydroxypropyl]-6-fluoro-2-(1-hydroxy-2-methylpropan-2-yl)-1Hindol-5-yl}cyclopropane-1-carboxamide. Its molecular formula is C26H27N2F3O6 and its molecular weight is 520.50. Tezacaftor has the following structural formula:
Ivacaftor
Ivacaftor is a white to off-white powder that is practically insoluble in water (<0.05 microgram/mL). Pharmacologically it is a CFTR potentiator. Its chemical name is N-(2,4-di-tert-butyl-5-hydroxyphenyl)-1,4-dihydro-4-oxoquinoline-3-carboxamide. Its molecular formula is C24H28N2O3 and its molecular weight is 392.49. Ivacaftor has the following structural formula:
Symdeko — Clinical Pharmacology
Mechanism of Action
Tezacaftor facilitates the cellular processing and trafficking of select mutant forms of CFTR (including F508del-CFTR) to increase the amount of mature CFTR protein delivered to the cell surface. Ivacaftor is a CFTR potentiator that facilitates increased chloride transport by potentiating the channel-open probability (or gating) of the CFTR protein at the cell surface. For ivacaftor to function CFTR protein must be present at the cell surface. Ivacaftor can potentiate the CFTR protein delivered to the cell surface by tezacaftor, leading to a further enhancement of chloride transport than either agent alone. The combined effect of tezacaftor and ivacaftor is increased quantity and function of CFTR at the cell surface, resulting in increases in chloride transport.
CFTR Chloride Transport Assay in Fischer Rat Thyroid (FRT) cells expressing mutant CFTR
The chloride transport response of mutant CFTR protein to tezacaftor/ivacaftor was determined in Ussing chamber electrophysiology studies using a panel of FRT cell lines transfected with individual CFTR mutations. Tezacaftor/ivacaftor increased chloride transport in FRT cells expressing CFTR mutations that result in CFTR protein being delivered to the cell surface.
The in vitro chloride transport response threshold was designated as a net increase of at least 10% of normal over baseline because it is predictive or reasonably expected to predict clinical benefit. For individual mutations, the magnitude of the net change over baseline in CFTR-mediated chloride transport in vitro is not correlated with the magnitude of clinical response.
Note that splice site mutations cannot be studied in the FRT assay.
Table 6 lists responsive CFTR mutations based on (1) a clinical FEV1 response and/or (2) in vitro data in FRT cells, indicating that tezacaftor/ivacaftor increases chloride transport to at least 10% of normal over baseline. CFTR gene mutations that are not responsive to ivacaftor alone are not expected to respond to Symdeko except for F508del homozygotes.
|
|||||
| 546insCTA | E92K | G576A | L346P | R117G | S589N |
| 711+3A→G* | E116K | G576A;R668C † | L967S | R117H | S737F |
| 2789+5G→A* | E193K | G622D | L997F | R117L | S912L |
| 3272-26A→G* | E403D | G970D | L1324P | R117P | S945L * |
| 3849+10kbC→T * | E588V | G1069R | L1335P | R170H | S977F* |
| A120T | E822K | G1244E | L1480P | R258G | S1159F |
| A234D | E831X | G1249R | M152V | R334L | S1159P |
| A349V | F191V | G1349D | M265R | R334Q | S1251N |
| A455E * | F311del | H939R | M952I | R347H * | S1255P |
| A554E | F311L | H1054D | M952T | R347L | T338I |
| A1006E | F508C | H1375P | P5L | R347P | T1036N |
| A1067T | F508C;S1251N † | I148T | P67L * | R352Q * | T1053I |
| D110E | F508del ‡ | I175V | P205S | R352W | V201M |
| D110H * | F575Y | I336K | Q98R | R553Q | V232D |
| D192G | F1016S | I601F | Q237E | R668C | V562I |
| D443Y | F1052V | I618T | Q237H | R751L | V754M |
| D443Y;G576A;R668C † | F1074L | I807M | Q359R | R792G | V1153E |
| D579G * | F1099L | I980K | Q1291R | R933G | V1240G |
| D614G | G126D | I1027T | R31L | R1066H | V1293G |
| D836Y | G178E | I1139V | R74Q | R1070Q | W1282R |
| D924N | G178R | I1269N | R74W | R1070W * | Y109N |
| D979V | G194R | I1366N | R74W;D1270N † | R1162L | Y161S |
| D1152H * | G194V | K1060T | R74W;V201M † | R1283M | Y1014C |
| D1270N | G314E | L15P | R74W;V201M;D1270N † | R1283S | Y1032C |
| E56K | G551D | L206W * | R75Q | S549N | |
| E60K | G551S | L320V | R117C * | S549R |
Pharmacodynamics
Effects on Sweat Chloride
In Trial 1 (patients age 12 years and older who were homozygous for the F508del mutation), the treatment difference between Symdeko and placebo in mean absolute change from baseline in sweat chloride through Week 24 was -10.1 mmol/L (95% CI: -11.4, -8.8).
In Trial 2 (patients age 12 years and older who were heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor), the treatment difference in mean absolute change from baseline in sweat chloride through Week 8 was -9.5 mmol/L (95% CI: -11.7, -7.3) between Symdeko and placebo, and -4.5 mmol/L (95% CI: -6.7, -2.3) between ivacaftor and placebo.
In Trial 4 (patients age 6 to less than 12 years) a reduction in sweat chloride was observed from baseline through Week 4 and sustained throughout the 24-week treatment period. Mean absolute change in sweat chloride from baseline through Week 24 was -14.5 mmol/L (95% CI: -17.4, -11.6).
Cardiac Electrophysiology
At a dose 3 times the maximum approved recommended dose, tezacaftor does not prolong the QT interval to any clinically relevant extent.
In a separate study of ivacaftor evaluating doses up to 3 times the maximum approved recommended dose, ivacaftor does not prolong the QT interval to any clinically relevant extent.
Pharmacokinetics
The pharmacokinetics of tezacaftor and ivacaftor are similar between healthy adult volunteers and patients with CF. Following once-daily dosing of tezacaftor and twice-daily dosing of ivacaftor in patients with CF, plasma concentrations of tezacaftor and ivacaftor reach steady-state within 8 days and within 3 to 5 days, respectively, after starting treatment. At steady-state, the accumulation ratio is approximately 1.5 for tezacaftor and 2.2 for ivacaftor. Exposures of tezacaftor (administered alone or in combination with ivacaftor) increase in an approximately dose-proportional manner with increasing doses from 10 mg to 300 mg once daily.
Key pharmacokinetic parameters for tezacaftor and ivacaftor at steady state are shown in Table 7.
| Drug | Cmax (mcg/mL) |
Effective t½ (h) |
AUC0-24h or AUC0-12h (mcg∙h/mL)* |
|
|---|---|---|---|---|
|
||||
| Tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours | Tezacaftor | 5.95 (1.50) | 15.0 (3.44) | 84.5 (27.8) |
| Ivacaftor | 1.17 (0.424) | 13.7 (6.06) | 11.3 (4.60) |
Absorption
After a single dose in healthy subjects in the fed state, tezacaftor was absorbed with a median (range) time to maximum concentration (tmax) of approximately 4 hours (2 to 6 hours). The median (range) tmax of ivacaftor was approximately 6 hours (3 to 10 hours) in the fed state.
When a single dose of tezacaftor/ivacaftor was administered with fat-containing foods, tezacaftor exposure was similar and ivacaftor exposure was approximately 3 times higher than when taken in a fasting state.
Distribution
Tezacaftor is approximately 99% bound to plasma proteins, primarily to albumin. Ivacaftor is approximately 99% bound to plasma proteins, primarily to alpha 1-acid glycoprotein and albumin. After oral administration of tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours in patients with CF in the fed state, the mean (±SD) for apparent volume of distribution of tezacaftor and ivacaftor was 271 (157) L and 206 (82.9) L, respectively. Neither tezacaftor nor ivacaftor partition preferentially into human red blood cells.
Elimination
After oral administration of tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours in patients with CF in the fed state, the mean (±SD) for apparent clearance values of tezacaftor and ivacaftor were 1.31 (0.41) and 15.7 (6.38) L/h, respectively. After steady-state dosing of tezacaftor in combination with ivacaftor in patients with CF, the effective half-lives of tezacaftor and ivacaftor were approximately 15 (3.44) and 13.7 (6.06) hours, respectively.
Metabolism
Tezacaftor is metabolized extensively in humans. In vitro data suggested that tezacaftor is metabolized mainly by CYP3A4 and CYP3A5. Following oral administration of a single dose of 100 mg 14C-tezacaftor to healthy male subjects, M1, M2, and M5 were the three major circulating metabolites of tezacaftor in humans. M1 has the similar potency to that of tezacaftor and is considered pharmacologically active. M2 is much less pharmacologically active than tezacaftor or M1, and M5 is not considered pharmacologically active. Another minor circulating metabolite, M3, is formed by direct glucuronidation of tezacaftor.
Ivacaftor is also metabolized extensively in humans. In vitro and in vivo data indicate that ivacaftor is metabolized primarily by CYP3A4 and CYP3A5. M1 and M6 are the two major metabolites of ivacaftor in humans. M1 has approximately one-sixth the potency of ivacaftor and is considered pharmacologically active. M6 is not considered pharmacologically active.
Excretion
Following oral administration of 14C-tezacaftor, the majority of the dose (72%) was excreted in the feces (unchanged or as the M2 metabolite) and about 14% was recovered in urine (mostly as M2 metabolite), resulting in a mean overall recovery of 86% up to 21 days after the dose. Less than 1% of the administrated dose was excreted in urine as unchanged tezacaftor, showing that renal excretion is not the major pathway of tezacaftor elimination in humans.
Following oral administration of ivacaftor alone, the majority of ivacaftor (87.8%) is eliminated in the feces after metabolic conversion. There was minimal elimination of ivacaftor and its metabolites in urine (only 6.6% of total radioactivity was recovered in the urine), and there was negligible urinary excretion of ivacaftor as unchanged drug.
Specific Populations
Based on population PK analyses, the PK exposure parameters of tezacaftor/ivacaftor in children and adolescents (ages 6 to <18 years) are similar to the AUCss range observed in adults when given in combination.
Pediatric patients age 6 to less than 12 years
| Age Group | Dose | tezacaftor AUCss mcg∙h/mL* |
ivacaftor AUCss mcg∙h/mL* |
|---|---|---|---|
|
|||
| 6 to <12 years † | 71.3 (28.3) | 8.5 (3.34) | |
| 6 to <12 years (<30 kg) | tezacaftor 50 mg/ ivacaftor 75 mg | 56.7 (22.3) | 6.92 (2.07) |
| 6 to <12 years (≥30 kg) † | tezacaftor 100 mg/ ivacaftor 150 mg | 92.7 (21.9) | 10.8 (3.52) |
Pediatric patients age 12 to less than 18 years
Following oral administration of Symdeko tablets, tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours, the mean (±SD) AUCss for tezacaftor and ivacaftor was 97.1 (35.8) mcg∙h/mL and 11.4 (5.50) mcg∙h/mL, respectively, similar to the mean AUCss in adult patients administered Symdeko tablets, tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours.
Patients with Hepatic Impairment
Following multiple doses of tezacaftor and ivacaftor for 10 days, patients with moderately impaired hepatic function (Child-Pugh Class B, score 7-9) had an approximately 36% increase in AUC and a 10% increase in Cmax for tezacaftor, and a 1.5-fold increase in ivacaftor AUC compared with healthy subjects matched for demographics. In a separate study, patients with moderately impaired hepatic function (Child-Pugh Class B, score 7-9) had similar ivacaftor Cmax, but an approximately 2.0-fold increase in ivacaftor AUC0-∞ compared with healthy subjects matched for demographics.
Pharmacokinetic studies have not been conducted in patients with mild (Child-Pugh Class A, score 5-6) or severe hepatic impairment (Child-Pugh Class C, score 10-15) receiving Symdeko. The magnitude of increase in exposure in patients with severe hepatic impairment is unknown but is expected to be higher than that observed in patients with moderate hepatic impairment [see Dosage and Administration (2.3), Use in Specific Populations (8.6), and Patient Counseling Information (17)].
Patients with Renal Impairment
Symdeko has not been studied in patients with moderate or severe renal impairment (creatinine clearance ≤30 mL/min) or in patients with end-stage renal disease. In a human pharmacokinetic study with tezacaftor alone, there was minimal elimination of tezacaftor and its metabolites in urine (only 13.7% of total radioactivity was recovered in the urine with 0.79% as unchanged drug).
In a human pharmacokinetic study with ivacaftor alone, there was minimal elimination of ivacaftor and its metabolites in urine (only 6.6% of total radioactivity was recovered in the urine).
In population pharmacokinetic analysis, data from 665 patients on tezacaftor or tezacaftor in combination with ivacaftor in clinical trials indicated that mild renal impairment (N=147; eGFR 60 to less than 90 mL/min/1.73 m2) and moderate renal impairment (N=7; eGFR 30 to less than 60 mL/min/1.73 m2) did not affect the clearance of tezacaftor significantly [see Use in Specific Populations (8.7)].
Male and Female Patients
The pharmacokinetic parameters of tezacaftor and ivacaftor are similar in males and females.
Drug Interactions Studies
Drug interaction studies were performed with Symdeko and other drugs likely to be co-administered or drugs commonly used as probes for pharmacokinetic interaction studies [see Drug Interactions (7)].
Potential for Tezacaftor/Ivacaftor to Affect Other Drugs
Clinical studies (with rosiglitazone and desipramine – see Table 9) showed that ivacaftor is not an inhibitor of CYP2C8 or CYP2D6. Based on in vitro results, ivacaftor has the potential to inhibit CYP3A and P-gp, and may also inhibit CYP2C9. In vitro, ivacaftor was not an inducer of CYP isozymes. Ivacaftor is not an inhibitor of transporters OATP1B1, OATP1B3, OCT1, OCT2, OAT1, or OAT3.
Based on in vitro results, tezacaftor has a low potential to inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP3A4. Tezacaftor has a low potential to induce CYP3A, but it is not an inducer of CYP1A2 and CYP2B6. Tezacaftor has a low potential to inhibit transporters P-gp, BCRP, OATP1B3, OCT2, OAT1, or OAT3.
Clinical studies with midazolam showed that Symdeko is not an inhibitor of CYP3A. Co-administration of Symdeko with digoxin, a sensitive P-gp substrate, increased digoxin exposure by 1.3-fold. Co-administration of Symdeko with an ethinyl estradiol/ norethindrone oral contraceptive had no significant effect on the exposures of the hormonal contraceptives. Co-administration of Symdeko with pitavastatin, an OATP1B1 substrate, had no clinically relevant effect on the exposure of pitavastatin.
The effects of tezacaftor and ivacaftor (or ivacaftor alone) on the exposure of co-administered drugs are shown in Table 9 [see Drug Interactions (7)].
Potential for Other Drugs to Affect Tezacaftor/Ivacaftor
In vitro studies showed that ivacaftor and tezacaftor were substrates of CYP3A enzymes (i.e., CYP3A4 and CYP3A5). Exposure to ivacaftor and tezacaftor will be reduced by concomitant CYP3A inducers and increased by concomitant CYP3A inhibitors.
In vitro studies showed that tezacaftor is a substrate for the uptake transporter OATP1B1, and efflux transporters P-gp and BCRP. Tezacaftor is not a substrate for OATP1B3. In vitro studies showed that ivacaftor is not a substrate for OATP1B1, OATP1B3, or P-gp.
The effects of co-administered drugs on the exposure of tezacaftor and ivacaftor (or ivacaftor alone) are shown in Table 10 [see Dosage and Administration (2.4) and Drug Interactions (7)].
| Dose and Schedule | Mean Ratio (90% CI) of Other Drugs No Effect=1.0 |
||||
|---|---|---|---|---|---|
| Drug | Dose | TEZ/IVA or IVA | Effect on Drug PK | AUC | Cmax |
| ↑ = increase, ↓ = decrease, ↔ = no change. CI = Confidence interval; TEZ = tezacaftor; IVA = ivacaftor; PK = Pharmacokinetics | |||||
|
|||||
| Midazolam | 2 mg single oral dose | TEZ 100 mg/IVA 150 mg every morning + IVA 150 mg every evening | ↔ Midazolam | 1.12 (1.01, 1.25) |
1.13 (1.01, 1.25) |
| Digoxin | 0.5 mg single dose | TEZ 100 mg/IVA 150 mg every morning + IVA 150 mg every evening | ↑ Digoxin | 1.30 (1.17, 1.45) |
1.32 (1.07, 1.64) |
| Oral Contraceptive | Ethinyl estradiol/ Norethindrone 0.035 mg/1.0 mg once daily |
TEZ 100 mg/IVA 150 mg every morning + IVA 150 mg every evening | ↔ Ethinyl estradiol | 1.12 (1.03, 1.22) |
1.15 (0.99, 1.33) |
| ↔ Norethindrone | 1.05 (0.98, 1.12) |
1.01 (0.87, 1.19) |
|||
| Pitavastatin | 2 mg single dose | TEZ 100 mg/IVA 150 mg every morning + IVA 150 mg every evening | ↑ Pitavastatin* | 1.24 (1.17, 1.31) |
0.977 (0.841, 1.14) |
| Rosiglitazone | 4 mg single oral dose | IVA 150 mg twice daily | ↔ Rosiglitazone | 0.975 (0.897, 1.06) |
0.928 (0.858, 1.00) |
| Desipramine | 50 mg single dose | IVA 150 mg twice daily | ↔ Desipramine | 1.04 (0.985, 1.10) |
1.00 (0.939; 1.07) |
| Dose and Schedule | Mean Ratio (90% CI) of Tezacaftor and Ivacaftor No Effect = 1.0 |
||||
|---|---|---|---|---|---|
| Drug | Dose | TEZ/IVA or IVA | Effect on TEZ/IVA PK | AUC | Cmax |
| ↑ = increase, ↓ = decrease, ↔ = no change. CI = Confidence interval; TEZ = tezacaftor; IVA = ivacaftor; PK = Pharmacokinetics | |||||
|
|||||
| Itraconazole | 200 mg twice a day on Day 1, followed by 200 mg once daily | TEZ 25 mg + IVA 50 mg once daily | ↑ Tezacaftor | 4.02 (3.71, 4.63) |
2.83 (2.62, 3.07) |
| ↑ Ivacaftor | 15.6 (13.4, 18.1) |
8.60 (7.41, 9.98) |
|||
| Ciprofloxacin | 750 mg twice daily | TEZ 50 mg + IVA 150 mg twice daily | ↔ Tezacaftor | 1.08 (1.03, 1.13) |
1.05 (0.99, 1.11) |
| ↑ Ivacaftor* | 1.17 (1.06, 1.30) |
1.18 (1.06, 1.31) |
|||
| Oral Contraceptive | Norethindrone/ethinyl estradiol 1.0 mg/0.035 mg once daily | TEZ 100 mg/IVA 150 mg every morning + IVA 150 mg every evening | ↔ Tezacaftor | 1.01 (0.963, 1.05) |
1.01 (0.933, 1.09) |
| ↔ Ivacaftor | 1.03 (0.960, 1.11) |
1.03 (0.941, 1.14) |
|||
| Rifampin | 600 mg once daily | IVA 150 mg single dose | ↓ Ivacaftor | 0.114 (0.097, 0.136) |
0.200 (0.168, 0.239) |
| Fluconazole | 400 mg single dose on Day 1, followed by 200 mg once daily | IVA 150 mg twice daily | ↑ Ivacaftor | 2.95 (2.27, 3.82) |
2.47 (1.93, 3.17) |
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies of carcinogenicity, mutagenicity, or impairment of fertility were conducted with the combination of tezacaftor and ivacaftor, however, separate studies of tezacaftor and ivacaftor are described below.
Tezacaftor
A 2-year study in Sprague-Dawley rats and a 6-month study in Tg.rasH2 transgenic mice were conducted to assess the carcinogenic potential of tezacaftor. No evidence of tumorigenicity from tezacaftor was observed in male and female rats at oral doses up to 50 and 75 mg/kg/day (approximately 2 and 3 times the MRHD based on summed AUCs of tezacaftor and its metabolites in males and females, respectively). No evidence of tumorigenicity was observed in male and female Tg.rasH2 transgenic mice at tezacaftor doses up to 500 mg/kg/day.
Tezacaftor was negative for genotoxicity in the following assays: Ames test for bacterial gene mutation, in vitro chromosomal aberration assay in Chinese hamster ovary cells, and in vivo mouse micronucleus test.
There were no effects on male or female fertility and early embryonic development in rats at oral tezacaftor doses up to 100 mg/kg/day (approximately 3 times the MRHD based on summed AUC of tezacaftor and M1 metabolite).
Ivacaftor
Two-year studies were conducted in CD-1 mice and Sprague-Dawley rats to assess the carcinogenic potential of ivacaftor. No evidence of tumorigenicity from ivacaftor was observed in mice or rats at oral doses up to 200 mg/kg/day and 50 mg/kg/day, respectively (approximately equivalent to 2 and 9 times the MRHD, respectively, based on summed AUCs of ivacaftor and its metabolites).
Ivacaftor was negative for genotoxicity in the following assays: Ames test for bacterial gene mutation, in vitro chromosomal aberration assay in Chinese hamster ovary cells, and in vivo mouse micronucleus test.
Ivacaftor impaired fertility and reproductive performance indices in male and female rats at 200 mg/kg/day (approximately 9 and 6 times, respectively, the MRHD based on summed AUCs of ivacaftor and its metabolites). Increases in prolonged diestrus were observed in females at 200 mg/kg/day. Ivacaftor also increased the number of females with all nonviable embryos and decreased corpora lutea, implantations, and viable embryos in rats at 200 mg/kg/day (approximately 6 times the MRHD based on summed AUCs of ivacaftor and its metabolites) when dams were dosed prior to and during early pregnancy. These impairments of fertility and reproductive performance in male and female rats at 200 mg/kg/day were attributed to severe toxicity. No effects on male or female fertility and reproductive performance indices were observed at ≤100 mg/kg/day (approximately 6 and 4 times, respectively, the MRHD based on summed AUCs of ivacaftor and its metabolites).
Clinical Studies
Dose Ranging:
Dose selection for the clinical program primarily consisted of one double-blind, placebo-controlled, multiple-cohort trial which included 176 patients with CF (homozygous for the F508del mutation) 18 years of age and older with a screening ppFEV1≥40. In the study, 34 and 106 patients, respectively, received tezacaftor at once-daily doses of 10 mg, 30 mg, 100 mg, or 150 mg alone or in combination with ivacaftor 150 mg q12h, and 33 patients received placebo. During the 28-day treatment period, dose-dependent increases in mean ppFEV1 change from baseline were observed with tezacaftor in combination with ivacaftor. Tezacaftor/ivacaftor in general had a greater mean treatment effect than tezacaftor alone. No additional benefit was observed at tezacaftor doses greater than 100 mg daily.
Efficacy:
The efficacy of Symdeko in patients with CF age 12 years and older was evaluated in three double-blind, placebo-controlled trials (Trials1, 2, and 3).
Trial 1 was a 24-week randomized, double-blind, placebo-controlled, two-arm study in patients with CF who were homozygous for the F508del mutation in the CFTR gene.
Trial 2 was a randomized, double-blind, placebo-controlled, 2-period, 3-treatment, 8-week crossover study in patients with CF who were heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor. Mutations predicted to be responsive were selected for the study based on the clinical phenotype (pancreatic sufficiency), biomarker data (sweat chloride), and in vitro responsiveness to tezacaftor/ivacaftor [see Clinical Studies (14.2)]. Patients were randomized to and received sequences of treatment that included Symdeko, ivacaftor, and placebo.
Trial 3 was a 12-week randomized, double-blind, placebo-controlled, two-arm study in patients with CF who were heterozygous for the F508del mutation and a second CFTR mutation predicted to be unresponsive to tezacaftor/ivacaftor. Mutations predicted to be non-responsive were selected for the study based on biologic plausibility (mutation class), clinical phenotype (pancreatic insufficiency), biomarker data (sweat chloride), and in vitro testing to tezacaftor and/or ivacaftor.
Patients in all trials continued on their standard-of-care CF therapies (e.g., bronchodilators, inhaled antibiotics, dornase alfa, and hypertonic saline) and were eligible to roll over into a 96-week open-label extension. Patients had a ppFEV1 at screening between 40-90%. Patients with a history of colonization with organisms associated with a more rapid decline in pulmonary status such as Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus, or who had 2 or more abnormal liver function tests at screening (ALT, AST, AP, GGT ≥3 × ULN or total bilirubin ≥2 × ULN) or AST or ALT ≥5 × ULN, were excluded from the trials.
Trial in Patients with CF Who Were Homozygous for the F508del Mutation in the CFTR Gene (Trial 1)
Trial 1 evaluated 504 patients (248 Symdeko, 256 placebo) with CF age 12 years and older (mean age 26.3 years). The mean ppFEV1 at baseline was 60.0% (range: 27.8% to 96.2%). The primary efficacy endpoint was change in lung function as determined by absolute change from baseline in ppFEV1 through Week 24. Treatment with Symdeko resulted in a statistically significant improvement in ppFEV1. The treatment difference between Symdeko and placebo for the mean absolute change in ppFEV1 from baseline through Week 24 was 4.0 percentage points (95% CI: 3.1, 4.8; P<0.0001). These changes persisted throughout the 24-week treatment period (Figure 2). Improvements in ppFEV1 were observed regardless of age, sex, baseline ppFEV1, colonization with Pseudomonas, concomitant use of standard-of-care medications for CF, and geographic region.
Key secondary efficacy variables included relative change from baseline in ppFEV1 through Week 24; number of pulmonary exacerbations from baseline through Week 24; absolute change in BMI from baseline at Week 24, and absolute change in CFQ-R Respiratory Domain Score (a measure of respiratory symptoms relevant to patients with CF, such as cough, sputum production, and difficulty breathing) from baseline through Week 24. For the purposes of this trial, a pulmonary exacerbation was defined as a change in antibiotic therapy (IV, inhaled, or oral) as a result of 4 or more of 12 pre-specified sino-pulmonary signs/symptoms. See Table 11 for a summary of key secondary outcomes in Trial 1.
| Placebo N=256 |
Symdeko N=248 |
||
|---|---|---|---|
| BMI: body mass index; CI: confidence interval; CFQ-R: Cystic Fibrosis Questionnaire-Revised; IVA: ivacaftor; NA: not applicable; ppFEV1: percent predicted forced expiratory volume in 1 second; | |||
|
|||
| Relative change in ppFEV1 from baseline through Week 24 (%) | Treatment difference (95% CI) | — | 6.8 (5.3, 8.3) |
| P value | NA | P<0.0001† | |
| Number of pulmonary exacerbations from baseline through Week 24 | Number of events (event rate per year‡) Rate ratio (95% CI) |
122 (0.99) | 78 (0.64) 0.65 (0.48, 0.88) |
| P value | NA | P=0.0054† | |
| Absolute change in BMI from baseline at Week 24 (kg/m2) | Treatment difference (95% CI) | — | 0.06 (-0.08, 0.19) |
| Absolute change in CFQ-R Respiratory Domain Score from baseline through Week 24 (points) | Treatment difference (95% CI) | — | 5.1 (3.2, 7.0) |
Figure 2: Absolute Change From Baseline in Percent Predicted FEV1 at Each Visit in Trial 1
Trial in Patients with CF Who Were Heterozygous for the F508del Mutation and a Second Mutation Predicted to be Responsive to Tezacaftor/Ivacaftor (Trial 2)
Trial 2 evaluated 244 patients with CF age 12 years and older (mean age 34.8 years). The mean ppFEV1 at baseline was 62.3% (range: 34.6 to 93.5). Of the 244 patients included in the efficacy analysis, 146 patients had a splice mutation and 98 patients had a missense mutation as the second allele. 161 patients received Symdeko, 156 patients received ivacaftor, and 161 patients received placebo. The primary efficacy endpoint was the mean absolute change from study baseline in percent predicted FEV1 averaged at Weeks 4 and 8 of treatment. The key secondary efficacy endpoint was absolute change in CFQ-R Respiratory Domain Score from study baseline averaged at Weeks 4 and 8 of treatment. For the overall population, treatment with Symdeko compared to placebo resulted in significant improvement in ppFEV1 (6.8 percentage points [95% CI: 5.7, 7.8]; P<0.0001) and CFQ-R Respiratory Domain Score (11.1 points (95% CI 8.7, 13.6); P<0.0001). Treatment difference for ppFEV1 between ivacaftor- and placebo-treated patients was 4.7 percentage points (95% CI: 3.7, 5.8; P<0.0001) and 2.1 percentage points (95% CI: 1.2, 2.9; P<0.0001) between Symdeko- and ivacaftor-treated patients, which were statistically significant. Improvements in ppFEV1 were observed regardless of age, baseline ppFEV1, sex, mutation class, colonization with Pseudomonas, concomitant use of standard-of-care medications for CF, and geographic region. Statistically significant improvements compared to placebo were also observed in the subgroup of patients with splice mutations and missense mutations (Table 12).
| Mutation (n) | Absolute Change in percent predicted FEV1*† | Absolute Change in CFQ-R Respiratory Domain Score (Points)*‡ | Absolute Change in Sweat Chloride (mmol/L)*‡ |
|---|---|---|---|
| (n=) patient numbers analysed | |||
|
|||
| Splice mutations (n= 93 for TEZ/IVA, n=97 for PBO) Results shown as difference in mean (95% CI) change from study baseline for Symdeko vs. placebo-treated patients: |
|||
| 7.4 (6.0, 8.7) | 9.5 (6.3, 12.7) | -5.4 (-8.0, -2.7) | |
| By individual splice mutation (n). Results shown as mean (minimum, maximum) for change from study baseline for Symdeko-treated patients | |||
| 2789+5G→A (25 ) | 8.6 (-1.5, 23.4) | 12.0 (-8.3, 38.9) | -3.2 (-16.5, 9.0) |
| 3272-26A→G (23) | 5.7 (-2.1, 25.9) | 5.7 (-22.2, 44.4) | -3.8 (-22.3, 16.5) |
| 3849+10kbC→T (43) | 5.8 (-7.2, 22.3) | 8.2 (-25.0, 47.2) | -5.6 (-27.0, 8.5) |
| 711+3A→G (2) | 4.3 (2.0, 6.7) | -4.2 (-5.6, -2.8) | -15.4 (-21.0, -9.8) |
| E831X§ (0) | NA | NA | NA |
| Missense mutations (n=66 for TEZ/IVA, n=63 for PBO) Results shown as difference in mean (95% CI) change from study baseline for Symdeko vs. placebo-treated patients: |
|||
| 5.9 (4.2, 7.5) | 13.4 (9.6, 17.3) | -16.3 (-19.7, -12.9) | |
| By individual missense mutation (n). Results shown as mean (minimum, maximum) for change from study baseline for Symdeko-treated patients | |||
| D579G (2) | 8.1 (-0.2, 16.4) | 11.1 (5.6, 16.7) | -23.1 (-24.8, -21.5) |
| D110H (1) | -1.0 (-1.0, -1.0) | -11.1 (-11.1, -11.1) | -22.5 (-22.5, -22.5) |
| D1152H (21) | 3.8 (-2.5, 12.5) | 15.2 (-8.3, 55.6) | -4.1 (-15.0, 11.5) |
| A455E (11) | 8.5 (2.6, 16.1) | 11.6 (-11.1, 44.4) | -0.3 (-8.8, 14.0) |
| L206W (4) | 3.0 (-4.5, 10.2) | 12.5 (-2.8, 38.9) | -36.1 (-44.5, -27.5) |
| P67L (11) | 9.4 (0.0, 31.9) | 11.7 (-12.5, 72.2) | -29.3 (-50.0, 0.8) |
| R1070W (2) | 6.1 (2.0, 10.1) | 29.2 (16.7, 41.7) | -13.8 (-26.8, -0.8) |
| R117C (1) | 2.9 (2.9, 2.9) | 16.7 (16.7, 16.7) | -38.8 (-38.8, -38.8) |
| R347H (2) | -0.5 (-2.8, 1.7) | 5.6 (-5.6, 16.7) | -13.8 (-19.0, -8.5) |
| R352Q (2) | 4.9 (2.6, 7.1) | 8.3 (8.3, 8.3) | -43.3 (-49.8, -36.8) |
| S945L (7) | 9.6 (0.7, 19.5) | 11.3 (-4.2, 25.0) | -29.0 (-42.5, -8.0) |
| S977F (2) | 10.1 (5.5, 14.7) | -1.4 (-8.3, 5.6) | -13.9 (-22.3, -5.5) |
In an analysis of BMI at Week 8, an exploratory endpoint, patients treated with Symdeko had a mean improvement of 0.2 kg/m2 (95% CI [0.0, 0.3]), 0.1 kg/m2 (95% CI [-0.1, 0.3]), and 0.3 kg/m2 (95% CI [0.1, 0.5]) versus placebo for the overall, splice, and missense mutation populations of patients, respectively.
Trial in Patients with CF Who Were Heterozygous for the F508del Mutation and a Second Mutation Not Predicted to be Responsive to Tezacaftor/Ivacaftor (Trial 3)
Trial 3 evaluated 168 patients with CF (83 Symdeko and 85 placebo) age 12 years and older (mean age 26.1 years) who were heterozygous for the F508del mutation and had a second CFTR mutation predicted to be unresponsive to tezacaftor/ivacaftor. CF patients with the F508del mutation and one of the following mutations in the CFTR gene were enrolled in the study (listed in decreasing frequency): W1282X, G542X, N1303K, 621+1G>T, 1717-1G>A, 1898+1G>A, CFTRdele2,3, 2183delAA>G, 2184insA, R1162X, R553X, 3659delC, 3905insT, G970R, I507del, R1066C, R347P, 1154insTC, 1811+1.6kbA>G, 2184delA, 405+1G>A, E60X, G85E, L1077P, Q39X, S466X, Y1092X, 1078delT, 1248+1G>A, 1677delTA, 1812-1G>A, 2869INSG, 3120+1G>A, 394delTT, 457TAT>G, 711+1G>T, 711+5G>A, 712-1G>T, G673x, L1065P, Q220X, Q493X, R709X, V520F. The mean ppFEV1 at baseline was 57.5% [range: 31.0 to 96.7]. The primary efficacy endpoint was change from baseline in absolute ppFEV1 through Week 12. The overall treatment difference between Symdeko and placebo for the mean absolute change in ppFEV1 from baseline through Week 12 was 1.2 percentage points (95% CI: -0.3, 2.6). This study was terminated following the planned interim analysis because the pre-specified futility criteria were met.
How Supplied/Storage and Handling
Symdeko (tezacaftor 50 mg/ivacaftor 75 mg fixed-dose combination tablet co-packaged with ivacaftor 75 mg tablet):
- Tezacaftor 50 mg/ivacaftor 75 mg fixed-dose combination tablets are supplied as white, capsule shaped tablets containing 50 mg of tezacaftor and 75 mg of ivacaftor. Each tablet is debossed with «V50» on one side and plain on the other.
- Ivacaftor 75 mg tablets are supplied as light blue, film-coated, capsule-shaped tablets containing 75 mg of ivacaftor. Each tablet is printed with the characters «V 75» on one side and plain on the other.
- 56-count tablet carton containing a 4-week supply (4 weekly wallets, each with 14 tablets) NDC 51167-113-01
Symdeko (tezacaftor 100 mg/ivacaftor 150 mg fixed-dose combination tablets co-packaged with ivacaftor 150 mg tablet):
- Tezacaftor 100 mg/ivacaftor 150 mg fixed-dose combination tablets are supplied as yellow, capsule-shaped tablets containing 100 mg of tezacaftor and 150 mg of ivacaftor. Each tablet is debossed with «V100» on one side and plain on the other.
- Ivacaftor 150 mg tablets are supplied as light blue, film-coated, capsule-shaped tablets containing 150 mg of ivacaftor. Each tablet is printed with the characters «V 150» on one side and plain on the other.
- 56-count tablet carton containing a 4-week supply (4 weekly wallets, each with 14 tablets) NDC 51167-661-01
Store at 68°F to 77°F (20°C to 25°C); excursions permitted to 59°F to 86°F (15°C to 30°C) [see USP Controlled Room Temperature].
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Transaminase (ALT or AST) Elevations and Monitoring
Inform patients that elevation in liver tests has occurred in patients treated with Symdeko or with ivacaftor alone. Transaminases (ALT and AST) should be assessed prior to initiating Symdeko, every 3 months during the first year of treatment, and annually thereafter. More frequent monitoring should be considered in patients with a history of transaminase elevations [see Warnings and Precautions (5.1)].
Drug Interactions with CYP3A Inducers and Inhibitors
Ask patients to tell you all the medications they are taking including any herbal supplements or vitamins. Co-administration of Symdeko with strong CYP3A inducers (e.g., rifampin, St. John’s wort) is not recommended, as they may reduce the therapeutic effectiveness of Symdeko. Adjustment of the dose to one tablet of tezacaftor/ivacaftor twice a week, taken approximately 3 to 4 days apart is recommended when co-administered with strong CYP3A inhibitors, such as ketoconazole. Advise the patient not to take the evening dose of ivacaftor. Dose reduction to one tablet of tezacaftor/ivacaftor or ivacaftor, taken on alternate days in the morning is recommended when co-administered with moderate CYP3A inhibitors, such as fluconazole. Advise the patient not to take the evening dose of ivacaftor. Food or drink containing grapefruit should be avoided [see Warnings and Precautions (5), Drug Interactions (7) and Clinical Pharmacology (12.3)].
Cataracts
Inform patients that abnormality of the eye lens (cataract) has been noted in some children and adolescents receiving Symdeko or with ivacaftor alone. Baseline and follow-up ophthalmological examinations should be performed in pediatric patients initiating treatment with Symdeko [see Warnings and Precautions (5.3)].
Use in Patients with Hepatic Impairment
Inquire and/or assess whether patients have liver impairment. Adjust the dose in patients with moderately impaired hepatic function (Child-Pugh Class B, score 7-9) to one tablet of tezacaftor/ivacaftor once daily in the morning and advise the patient not to take the evening dose of ivacaftor. Symdeko has not been studied in patients with severe hepatic impairment (Child-Pugh Class C, score 10-15); however, exposure is expected to be substantially higher than that observed in patients with moderate hepatic impairment. When benefits are expected to outweigh the risks, Symdeko should be used with caution in patients with severe hepatic impairment at a dose of one tablet of tezacaftor/ivacaftor once daily in the morning or less frequently. Advise the patient not to take the evening dose of ivacaftor. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh Class A, score 5-6) [see Dosage and Administration (2.3), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
Administration
Inform patients that Symdeko is best absorbed by the body when taken with food that contains fat. A typical CF diet will satisfy this requirement. Examples include eggs, butter, peanut butter, cheese pizza, whole-milk dairy products (such as whole milk, cheese, and yogurt), etc. [see Dosage and Administration (2.1) and Clinical Pharmacology (12.3)].
Patients should be informed about what to do in the event they miss a dose of Symdeko or ivacaftor:
- If 6 hours or less have passed since the time Symdeko is usually taken, patients should be instructed to take the prescribed dose of Symdeko with fat-containing food as soon as possible.
- If more than 6 hours have passed since the time Symdeko is usually taken, the missed dose should NOT be taken and the patient should resume the usual dosing schedule.
- Patients should be advised to contact their health care provider if they have questions.
Manufactured for
Vertex Pharmaceuticals Incorporated
50 Northern Avenue
Boston, MA 02210
Approved June 2022
Symdeko, VERTEX and the VERTEX triangle logo are registered trademarks of Vertex Pharmaceuticals Incorporated.
All other trademarks referenced herein are the property of their respective owners.
©2022 Vertex Pharmaceuticals Incorporated
ALL RIGHTS RESERVED
Patient Information is perforated for dispensing to the patient.
| PATIENT INFORMATION Symdeko (SIM-deh-koh) (tezacaftor/ivacaftor tablets; ivacaftor tablets) for oral use |
||||
What is Symdeko?
It is not known if Symdeko is safe and effective in children under 6 years of age. |
||||
Do not take Symdeko if you take certain medicines or herbal supplements such as:
Talk to your doctor before taking Symdeko if you take any of the medicines or herbal supplements listed above. |
||||
Before taking Symdeko, tell your doctor about all of your medical conditions, including if you:
Symdeko may affect the way other medicines work, and other medicines may affect how Symdeko works.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine. |
||||
How should I take Symdeko?
|
||||
What should I avoid while taking Symdeko?
|
||||
| What are the possible side effects of Symdeko? Symdeko can cause serious side effects, including:
Your doctor may do blood tests to check the liver more often if you have had high liver enzymes in your blood in the past. |
||||
|
|
|||
The most common side effects of Symdeko include: |
||||
|
|
|||
| These are not all the possible side effects of Symdeko. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
How should I store Symdeko?
Keep Symdeko and all medicines out of the reach of children. |
||||
| General information about the safe and effective use of Symdeko. Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Symdeko for a condition for which it was not prescribed. Do not give Symdeko to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or doctor for information about Symdeko that is written for health professionals. |
||||
| What are the ingredients in Symdeko? tezacaftor/ivacaftor tablets: Active ingredients: tezacaftor and ivacaftor Inactive ingredients: hypromellose acetate succinate, sodium lauryl sulfate, hypromellose, microcrystalline cellulose, croscarmellose sodium, magnesium stearate, HPMC/hypromellose 2910, hydroxypropyl cellulose, titanium dioxide, talc, and iron oxide yellow (in tezacaftor 100 mg/ivacaftor 150 mg tablets only). ivacaftor tablets: Active ingredients: ivacaftor Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, lactose monohydrate, magnesium stearate, microcrystalline cellulose, sodium lauryl sulfate, carnauba wax, FD&C Blue #2, PEG 3350, polyvinyl alcohol, talc, titanium dioxide, ammonium hydroxide, iron oxide black, propylene glycol, and shellac. |
||||
|
|
||||
| Manufactured for: Vertex Pharmaceuticals Incorporated; 50 Northern Avenue, Boston, MA 02210 Symdeko, VERTEX and the VERTEX triangle logo are registered trademarks of Vertex Pharmaceuticals Incorporated. All other trademarks referenced herein are the property of their respective owners. ©2019 Vertex Pharmaceuticals Incorporated For more information, go to www.Symdeko.com or call 1-877-752-5933. |
||||
| This Patient Information has been approved by the U.S. Food and Drug Administration. | Approved December2020 | |||
PRINCIPAL DISPLAY PANEL — Kit Carton
Rx Only
NDC 51167-661-01
Symdeko®
(tezacaftor/ivacaftor) 100 mg/150 mg
and (ivacaftor) 150 mg tablets
56 tablets
Contains 4-week supply of Symdeko
4 weekly blister cards, each with 14 tablets:
(7 tezacaftor/ivacaftor and 7 ivacaftor tablets)
LIFT HERE TO OPEN ▶
PRINCIPAL DISPLAY PANEL — Kit Carton — 113
Rx Only
NDC 51167-113-01
Symdeko®
(tezacaftor/ivacaftor) 50 mg/75 mg
and (ivacaftor) 75 mg tablets
56 tablets
Contains 4-week supply of Symdeko
4 weekly blister cards, each with 14 tablets:
(7 tezacaftor/ivacaftor and 7 ivacaftor tablets)
LIFT HERE TO OPEN ▶
| Symdeko tezacaftor and ivacaftor kit |
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
| Symdeko tezacaftor and ivacaftor kit |
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
|
Labeler — Vertex Pharmaceuticals Incorporated (602478257)
Vertex Pharmaceuticals Incorporated
Frequently asked questions
- How do the warnings differ between Symdeko and Orkambi?
- Can you take Symdeko with birth control pills?
- How are Symdeko tablets taken?
- How does Symdeko work?
- What is the difference between Symdeko and Orkambi?
- What is the difference between Symdeko and Kalydeco?
View more FAQ
Medical Disclaimer
Коротко
«Вертекс фармасьютикалс» (Vertex Pharmaceuticals) получила разрешение Управления по санитарному надзору за качеством пищевых продуктов и медикаментов США (FDA) на «Симдеко» (Symdeko, тезакафтор + ивакафтор, ивакафтор) — новый препарат для терапии муковисцидоза у пациентов 12 лет и старше, заболевание которых характеризуется гомозиготной (две копии) мутацией F508del или хотя бы одной мутацией гена муковисцидозного трансмембранного регулятора проводимости (CFTR), которая отвечает на назначение лекарства.
Текущий список CFTR-мутаций, при которых «Симдеко» подтвержденно срабатывает, включает следующие: F508del/F508del, 711+3A→G, 2789+5G→A, 3272-26A→G, 3849+10kbC→T, A455E, A1067T, D110E, D110H, D579G, D1152H, D1270N, E56K, E193K, E831X, F1052V, F1074L, K1060T, L206W, P67L, R74W, R117C, R347H, R352Q, R1070W, S945L, S977F.
«Симдеко» стал третьим противомуковисцидозным медикаментом «Вертекс» — после «Калидеко» (Kalydeco, ивакафтор) и «Оркамби» (Orkambi, лумакафтор + ивакафтор), которые были одобрены в январе 2012 года и июле 2015-го соответственно.
Подробности
Тезакафтор (tezacaftor), будучи CFTR-корректором (модулятором), способствует клеточному процессингу и миграции нормальных и определенных мутантных форм CFTR (включая F508del-CFTR) в целях увеличения количества зрелого CFTR-белка, доставляемого к клеточной поверхности. Ивакафтор (ivacaftor) является CFTR-усилителем (потенциатором), повышающим вероятность открытия ионного канала CFTR-белка, чтобы ионы хлора могли пройти через него. Для работы ивакафтора необходимо, чтобы CFTR-белок располагался на клеточной поверхности — этому как раз и содействует тезакафтор.

В Европе «Симдеко» будет одобрен, как ожидается, во втором полугодии.

Другими словами, «Вертекс» и дальше желает наращивать финансовые показатели. Так, если в 2016 году компания заработала на «Калидеко» и «Оркамби» 1,68 млрд долларов, то в 2017-м они принесли 2,17 млрд долларов. Между тем «Вертекс» тратит, пожалуй, больше всех в фармотрасли денег на научно-исследовательские проекты: в прошлом году она пустила на НИОКР где-то 55% финансов, поступивших от продаж лекарств.
Согласно прогнозам отраслевых экспертов, в 2018 году доходы «Вертекс» составят 2,84 млрд долларов, в 2019-м они вырастут до 3,75 млрд долларов.
Идефикс «Вертекс» — сделать лекарства, которые подходили бы для 90% больных муковисцидозом. Нынешние медикаменты помогают лишь 40% пациентов. Проблема обусловлена изобилием различных мутаций CFTR, которых насчитывается приблизительно 2 тыс. Вот почему компания упорно разрабатывает CFTR-корректоры следующего поколения. В ближайшем будущем должна появиться прорывная терапия муковисцидоза, включающая три компонента.
Важная информация
Mosmedpreparaty.ru — специализированная научно-исследовательская и справочно-информационная аналитическая служба группы компаний «Мосмедпрепараты», таргетированная на ключевые события глобальной отрасли фармации, биотехнологий, медицины и здравоохранения.
- Ничто на Mosmedpreparaty.ru не является рекламой или продвижением лекарственных препаратов, методов лечения, медицинских услуг.
- Сведения и публикации Mosmedpreparaty.ru носят исключительно научно-просветительский и ознакомительный характер.
- Медицинская информация, транслируемая Mosmedpreparaty.ru, предназначена только для специалистов в области здравоохранения и сфере обращения лекарственных средств.
- Медицинская информация, содержащаяся на Mosmedpreparaty.ru, не предназначена для использования в качестве замены консультации со специалистом в области здравоохранения.
- Ничто на Mosmedpreparaty.ru не должно истолковываться как предоставление медицинского совета или рекомендации и не может служить основанием для принятия каких-либо решений или осуществления каких-либо действий без участия специалиста в области здравоохранения.
Присутствие на веб-ресурсе Mosmedpreparaty.ru и ознакомление с его содержимым означает, что вы прочитали «Пользовательское соглашение» и приняли его условия.
Войти

|
Муковисцидоз представляет собой серьезное генетическое Эффективность препарата Симдеко у пациентов с муковисцидозом Лекарственное средство всегда следует принимать с пищей, Источник: fda.gov
|

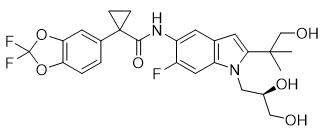
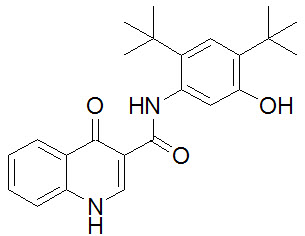
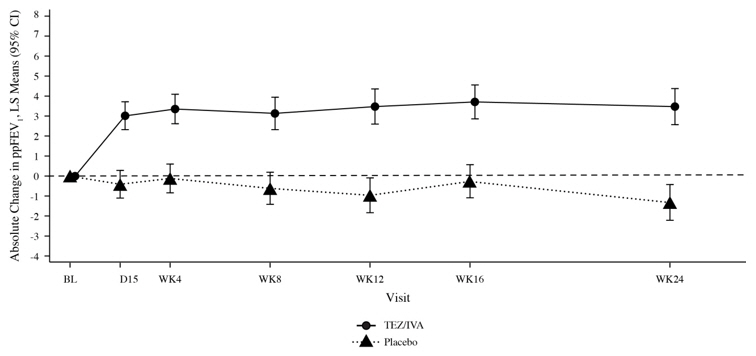


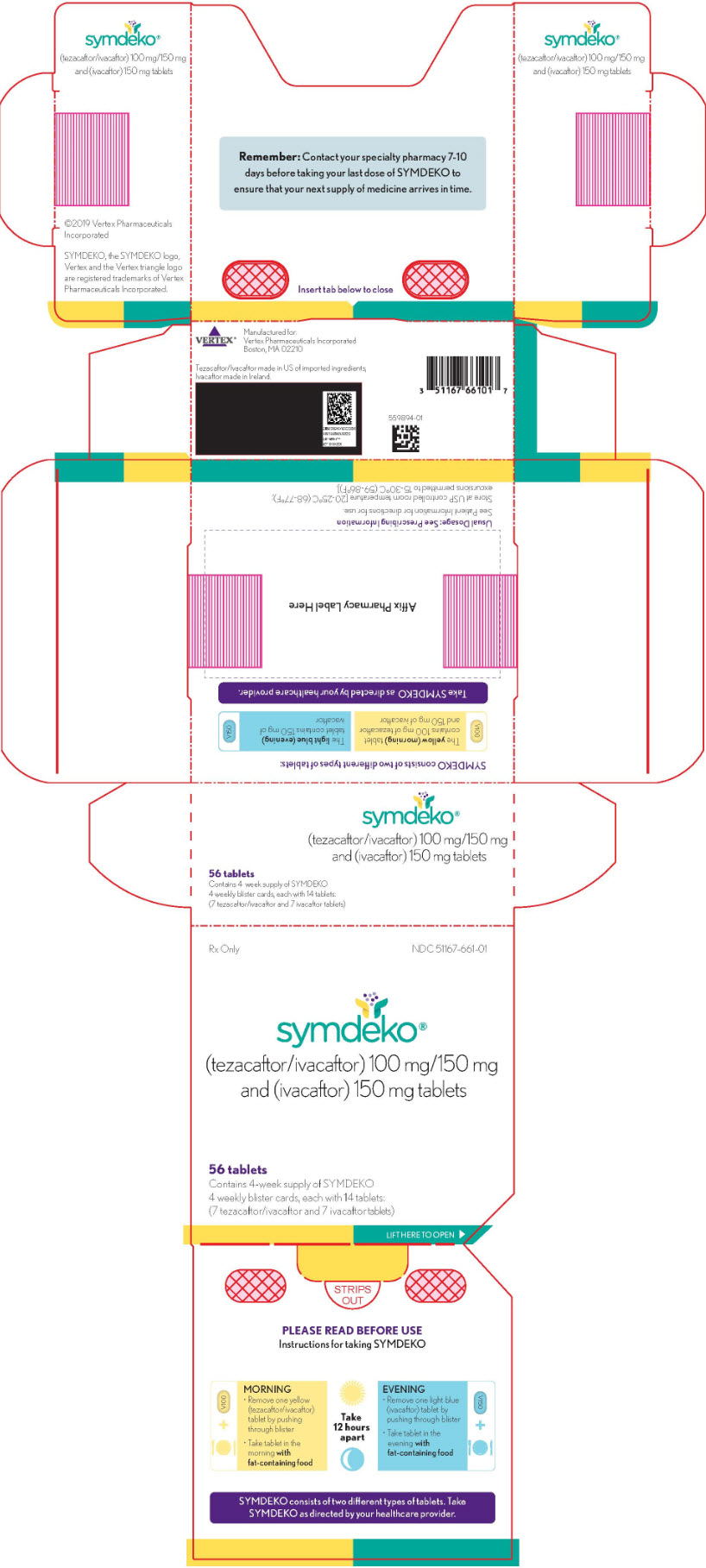
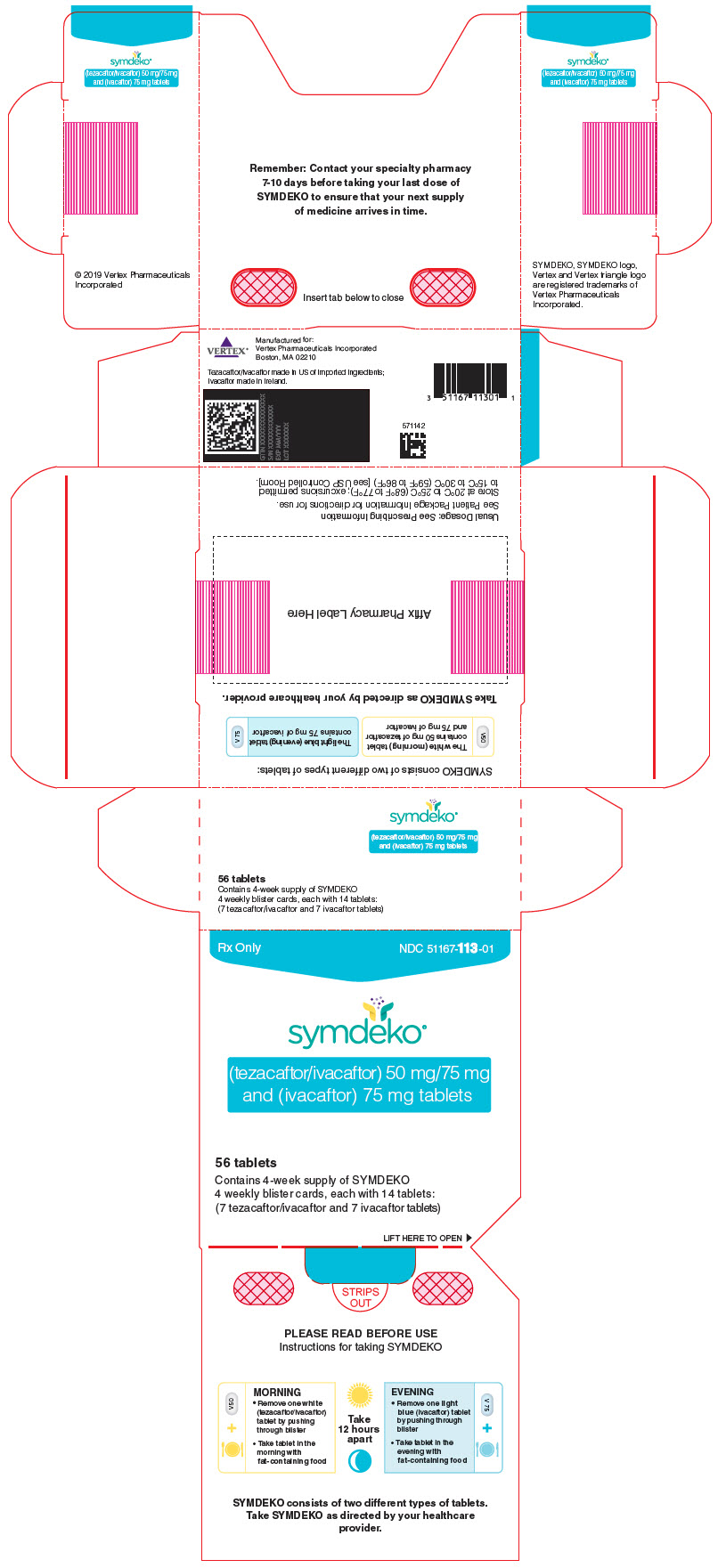

 FDA одобрило расширение показаний к применению препарата
FDA одобрило расширение показаний к применению препарата